Temperance in Antibiotic Usage
- 6/13/16
[vc_column css=".vc_custom_1501598298455{padding-right: 0px !important;padding-left: 0px !important;}"][vc_column_text el_id="text-content"]Dr. Martin Blaser, author of the book Missing Microbes, recently penned a thought-provoking editorial in the journal Science, entitled Antibiotic use and its consequences for the normal microbiome.
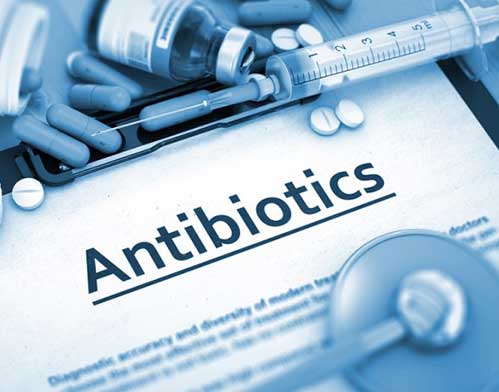
Dr. Blaser begins by confirming the important positive role that antibiotics play in modern medicine. He then reiterates the words of Nobel laureate Alexander Fleming, discoverer of penicillin, who in 1945 warned of the potential consequences of antibiotics, including the development of antibiotic resistant organisms.
He then goes on to review how, shortly after their introduction for widespread use in humans, farmers discovered that treating livestock with antibiotics dramatically enhanced their growth. This discovery fostered the widespread use of antibiotics in the livestock industry that has persisted over the last six decades. But beyond the historical significance of this discovery, the report calls attention to the fact that antibiotics are associated with important metabolic changes. And this was one of the central ideas elucidated in Dr. Blaser’s book, wherein he linked current antibiotic mismanagement to the global, ever-increasing rates of overweight and obesity.
The editorial then reveals the link between antibiotic exposure and risk for a variety of common diseases including obesity, types 1 and 2 diabetes, inflammatory bowel diseases, celiac disease, allergies and asthma. Importantly, Dr. Blaser makes it clear that current scientific research validates that the relationship between antibiotic exposure and these diseases is not just correlative, but causal, and clearly related, mechanistically, to changes in the makeup of the microbiome.
Loss of species diversity is a hallmark of antibiotic induced microbiome disruption, and the report graphically demonstrates strong correlation between antibiotic usage and other sanitation practices with this change when comparing populations that experienced “early modernization” with those in which these practices were comparatively delayed.
Animal and human research make it clear that the most dramatic effects of antibiotic exposure, both in terms of microbiome alteration as well as risk for various disease conditions as a consequence of these changes, occur when the drugs are administered in early life. Thus, Dr. Blaser councils,
“Rather than carpet-bombing germs into submission with broad-spectrum antibiotics, we will need more laser-like approaches to develop drugs against specific pathogens, minimize damage to essential symbiotic microbial species and preserve community structure and function in the healthy (and developing) microbiome. “
He then poses several important questions, asking,
“There always will be instances in which children must be treated with an antibiotic, but the collateral effects could be mitigated. Should we bank every healthy child’s fecal specimen, so we can chase each antibiotic course with a dose of their own pretreatment microbiota? Or by studying microbiota before and after antibiotic treatment, can we identify a few key organisms to replace in that child and then prescribe well-characterized pharmaceutical-grade standard strains, the probiotics of the future, to be administered in the appropriate vehicle?”
Antibiotic usage continues to expand at an alarming rate. During the decade 2000 and 2010, total global antibiotic consumption grew by more than 30 percent. Again, these are profoundly useful medications. But as Dr. Blaser reminds us:
“Yet antibiotics are vital for health care. It is difficult to imagine optimal health without an umbrella of antibiotics to use when needed. Nevertheless, practitioners have not been taking the biologic cost of antibiotic use into account sufficiently in making treatment decisions.”
With our new understanding of the profound microbiome-induced metabolic consequences brought on by antibiotic exposure, and the myriad diseases that result from these changes, we are now called upon to reassess our decision process based upon the risk-benefit ratio of this important, but clearly over-utilized class of medicines.[vc_column width="1/4"][vc_single_image image="73" img_size="medium" alignment="center"][vc_column width="3/4"][vc_empty_space height="5px"][vc_column_text]About Dr. Perlmutter: David Perlmutter, M.D., is an expert in the human microbiome, a board-certified neurologist, Fellow of the American College of Nutrition, America’s brain-health expert and #1 New York Times best-selling author.[vc_column][vc_column_text]This information is intended for educational and informational purposes only. It should not be used in place of an individual consultation or examination or replace the advice of your health care professional and should not be relied upon to determine diagnosis or course of treatment.
Dr. Blaser begins by confirming the important positive role that antibiotics play in modern medicine. He then reiterates the words of Nobel laureate Alexander Fleming, discoverer of penicillin, who in 1945 warned of the potential consequences of antibiotics, including the development of antibiotic resistant organisms.
He then goes on to review how, shortly after their introduction for widespread use in humans, farmers discovered that treating livestock with antibiotics dramatically enhanced their growth. This discovery fostered the widespread use of antibiotics in the livestock industry that has persisted over the last six decades. But beyond the historical significance of this discovery, the report calls attention to the fact that antibiotics are associated with important metabolic changes. And this was one of the central ideas elucidated in Dr. Blaser’s book, wherein he linked current antibiotic mismanagement to the global, ever-increasing rates of overweight and obesity.
The editorial then reveals the link between antibiotic exposure and risk for a variety of common diseases including obesity, types 1 and 2 diabetes, inflammatory bowel diseases, celiac disease, allergies and asthma. Importantly, Dr. Blaser makes it clear that current scientific research validates that the relationship between antibiotic exposure and these diseases is not just correlative, but causal, and clearly related, mechanistically, to changes in the makeup of the microbiome.
Loss of species diversity is a hallmark of antibiotic induced microbiome disruption, and the report graphically demonstrates strong correlation between antibiotic usage and other sanitation practices with this change when comparing populations that experienced “early modernization” with those in which these practices were comparatively delayed.
Animal and human research make it clear that the most dramatic effects of antibiotic exposure, both in terms of microbiome alteration as well as risk for various disease conditions as a consequence of these changes, occur when the drugs are administered in early life. Thus, Dr. Blaser councils,
“Rather than carpet-bombing germs into submission with broad-spectrum antibiotics, we will need more laser-like approaches to develop drugs against specific pathogens, minimize damage to essential symbiotic microbial species and preserve community structure and function in the healthy (and developing) microbiome. “
He then poses several important questions, asking,
“There always will be instances in which children must be treated with an antibiotic, but the collateral effects could be mitigated. Should we bank every healthy child’s fecal specimen, so we can chase each antibiotic course with a dose of their own pretreatment microbiota? Or by studying microbiota before and after antibiotic treatment, can we identify a few key organisms to replace in that child and then prescribe well-characterized pharmaceutical-grade standard strains, the probiotics of the future, to be administered in the appropriate vehicle?”
Antibiotic usage continues to expand at an alarming rate. During the decade 2000 and 2010, total global antibiotic consumption grew by more than 30 percent. Again, these are profoundly useful medications. But as Dr. Blaser reminds us:
“Yet antibiotics are vital for health care. It is difficult to imagine optimal health without an umbrella of antibiotics to use when needed. Nevertheless, practitioners have not been taking the biologic cost of antibiotic use into account sufficiently in making treatment decisions.”
With our new understanding of the profound microbiome-induced metabolic consequences brought on by antibiotic exposure, and the myriad diseases that result from these changes, we are now called upon to reassess our decision process based upon the risk-benefit ratio of this important, but clearly over-utilized class of medicines.[vc_column width="1/4"][vc_single_image image="73" img_size="medium" alignment="center"][vc_column width="3/4"][vc_empty_space height="5px"][vc_column_text]About Dr. Perlmutter: David Perlmutter, M.D., is an expert in the human microbiome, a board-certified neurologist, Fellow of the American College of Nutrition, America’s brain-health expert and #1 New York Times best-selling author.[vc_column][vc_column_text]This information is intended for educational and informational purposes only. It should not be used in place of an individual consultation or examination or replace the advice of your health care professional and should not be relied upon to determine diagnosis or course of treatment.